NEONATAL GROWTH AND MATURITY
Until recently, the only factor used to determine developmental age of the newborn, was weight. Today, the gestational age is determined, in order to assess the maturity of the infant.
These are three methods used to assess neonatal growth and maturity:
- Duration of the pregnancy as computed from the onset of the mother’s last menstrual period and other obstetrical data
- Growth as determined by birth weight and size of infant
- Maturity physical and neurological development of the infant
GESTATIONAL AGE FROM OBSTETRICAL INFORMATION
The first of the three categories is gestational age, and is the most frequently used and obtained from obstetrical records. There are situations where this is inaccurate, but most often the date of last menstrual period is used. Fertilization occurs approximately 2 weeks after the onset of the LMP (last menstrual period).
From this fertilization date, the “normal” newborn gestation period is about forty weeks. 38 weeks to 42 weeks is also considered normal. Infants born before the completion of the 37th week are “preterm”. Those born after the 42nd week are “post term”.
Examinations of the amniotic fluid, ultrasonic measurements and fundal height may help to indicate gestational age when the LMP is not precisely known. These items however, are not accurate and will be used in conjunction with any other data available.
ASSESSMENT OF GROWTH
The following three items are widely used to determine the physical growth of the infant in relation to the gestational period of the infant. These items can be affected by other circumstances. Genetic differences can affect these; as well as can: diabetes, anomalies, drugs, prenatal care, and many other factors. It will be pointed out that since there are many factors that influence physical characteristics of the infant, all factors must be considered before calling an infant “at-risk” by saying he/she is premature.
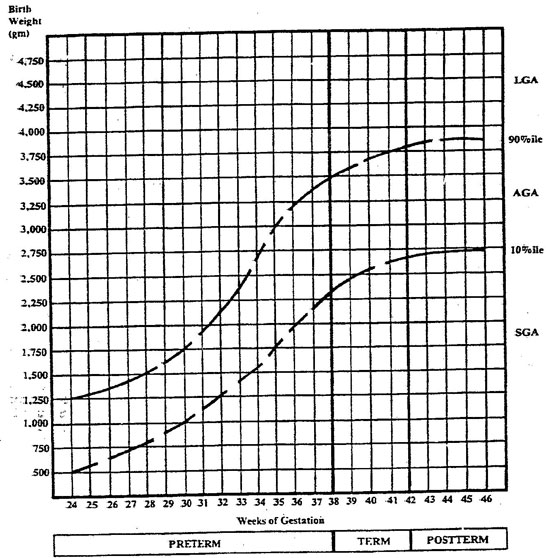
- Birth Weight
SGA, Small for Gestational Age, at 40 weeks less than 2500 Grams
LGA, Large for Gestational Age, at 40 weeks more than 3750 Grams
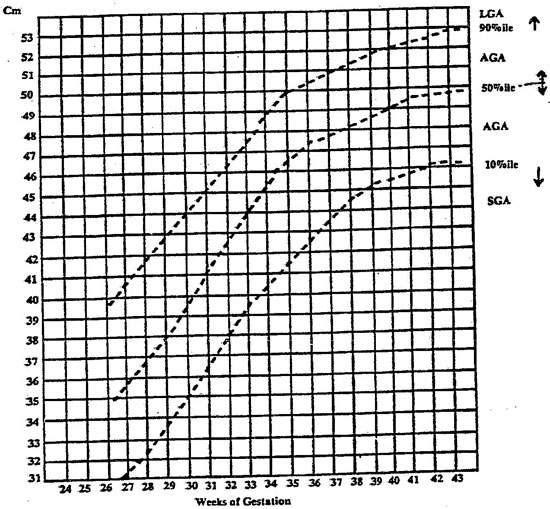
- Length
Assess crown to heel length in centimeters
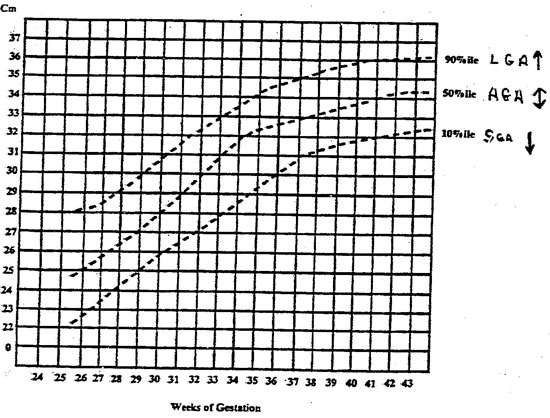
- Head Circumference
Assess frontal-occipital circumference
ASSESSMENT OF MATURITY
The following section will present a reference guide for assessing the maturity of the infant. This maturity can be correlated to the infant’s gestational age which we have already discussed. According to Korones, an infant should reach an acceptable level of physical maturity by a certain gestational age. After we have presented all assessments to be made, we will present the level of growth which the newborn should attain by birth.
Physical Assessment:
- after birth record: date and time of birth
- gestational age (according the LMP method)
- weight in Grams
- Apgar scores at 1 minute and 5 minutes
There are a number of assessment procedures for determining the assessment of maturity.
These are the guidelines for assessment by Dubowitz:
- presence or absence of edema
- skin texture and color and opacity
- presence or absence of lanugo
- plantar creases
- nipple formation
- breast size
- ear form and firmness
- genitals
All of these items can be significant when the physician determines the maturity of the infant. Most nurses will not normally conduct this in-depth assessment. However, your findings may be very helpful to the final determination of the infant’s maturity. Your hospital may use a different scale, but they all are essentially the same.
NEUROLOGICAL ASSESSMENT
The following assessment data will be used in conjunction with information previously obtained, in order to determine the maturity of the infant. If the infant is found to be under-developed or over-developed, the infant might be at-risk for certain special types of disorders of maturity. It may mean that there is a congenital deformity which has not surfaced yet. The guide we are presenting may be different from the one used at your facility; always use your hospital’s procedure. If you have further questions, you may use any basic pediatrics or obstetrical nursing textbook for further details.
- Posture
Normal newborn flexes both arms and legs when lying quiet and supine
- Square Window
The normal newborn’s hand and wrist will flex greatly, so that the angle between hand and forearm is very low (30 degrees or less)
- Ankle Dorsiflexion
Same as above, when gently flexed by the examiner, the angle between dorsum of foot and leg is very low (30 degrees or less) (extreme flexion is possible)
- Arm Recoil
Normal newborns will recoil their arm about half way or up to 90 degrees after the arm is flexed at the elbow by the examiner for at least 5 seconds. Then after fully extending the arm by pulling on the hand, the infant’s arm should recoil; be sure infant is supine.
- Leg Recoil
Similar to above, when the infant’s hips are flexed by examiner and then pulled out straight, they will partially recoil (up to about 90 degrees)
- Popliteal Angle
Similar to above, start with infant’s thigh flexed in the knee-chest position, and leave it there by holding it gently. Now extend the lower leg as much as possible and let it go. The lower leg should return and form an angle of about 90 degrees.
- Heel-to-Ear Maneuver
In the supine position, extend the foot as close as possible to the infant’s head. Note the angle of the knee (lower leg and thigh), it should be about 90 degrees or slightly higher angle
- Head lag
Start infant in supine position and begin to pull to a sitting position by grasping both hands. If the head is supported by the infant in an even plane with the rest of the body, the infant is normal. The head should not “lag” behind for any period of time.
- Ventral suspension
Suspend the infant in the prone position with a hand (or tow) under the infant’s chest. In the normal infant, the back should be only slightly arched and the arms and legs should be held by the infant at an angle to the body, with elbows and knees flexed. (If dropped down, would be in a crawling position).
This was a detailed assessment that the nurse can perform or assist with. Record all findings, especially if abnormal. All of these neuro tests will show that the normal newborn infant should have a certain amount of neuro-muscular control over its body, even immediately after birth. The tests here should be performed when the infant is at rest. If crying, the tests may not be valid. If the infant over-reacts or under-reacts, it may mean that the infant is over or under developed for its gestational age. If the infant does not react normally, remember that it may be only a variation of normal. If there are grossly abnormal findings, report them immediately.
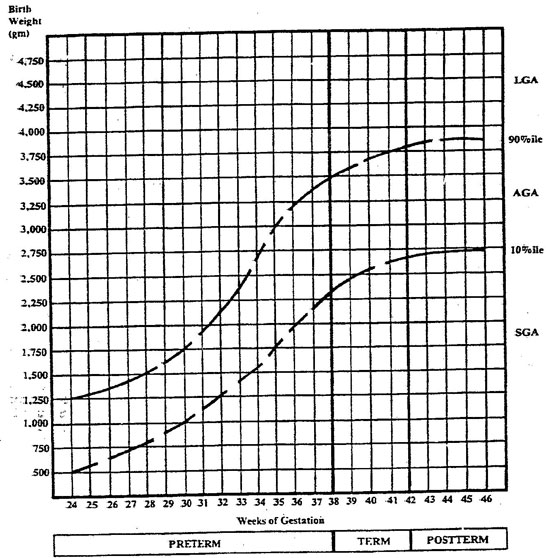
Figure 1. Classification of newborns by birth weight and gestational age.
Note. Adapted from “Neonatal Mortality Rate: Relationship to Birth Weight and Gestational Age” by L.O. Lubchenco, D.T.
Searls, & J.V. Brazic, “The Journal of Pediatrics”, October 1972, 814-822. Copyright 1972 by C.V. Mosby. Reprinted by permission
This form may be reproduced. The March of Dimes Birth Defects Foundation, 1982
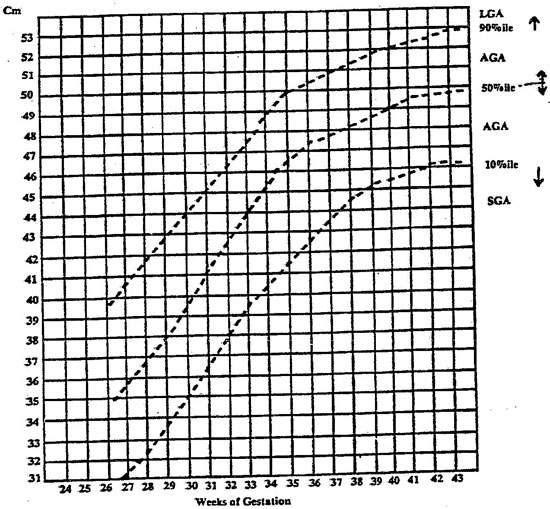
Figure 2. Classification of newborns by length and gestational age.
Note. Adapted from “Intrauterine Growth in Length and Head Circumference as Estimated from Live Births at Gestation Ages from 26 to 42
Weeks” by L.O. Lubchenco, C. Hansman, and E. Boyd, Pediatrics, 1966, 37(3), 403-416. Copyright 1966 by the American Academy of Pediatrics.
Reprinted with permission.
This form may be reproduced. The March of Dimes Birth Defects Foundation, 1982.
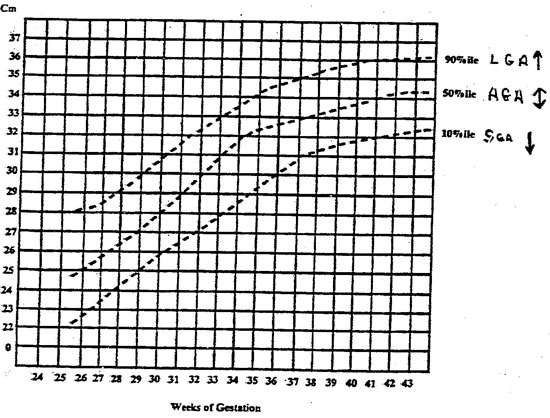
Figure 3. Classification of newborns by head circumference and gestational age.
Note. Adapted from “Intrauterine Growth in Length and Heaf Circumference as Estimated from Live Births at Gestational Ages from 26 to 42”
Weeks. By L.O. Lubchenco, C. Hansman, and E. Boyd, Pediatrics, 1966, 37(3), 403-416. Copyright 1966 by the American Academy of Pediatrics.
Reprinted with permission.
This form may be reproduced. The March of Dimes Birth Defects Foundation, 1982.
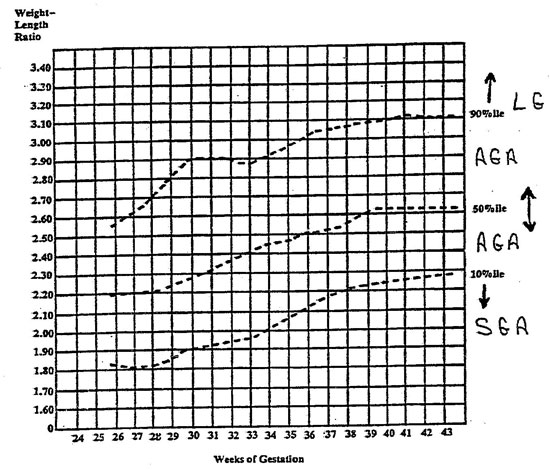
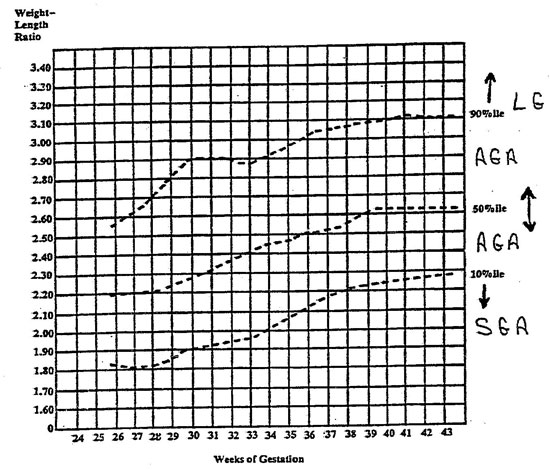
Figure 4. Classification of newborns by weight-length ratio and gestational age.
Note. Adapted from “Intrauterine Growth in Length and Head Circumference as Estimated from Live Births at Gestational Ages from 26 to 42
Weeks” by L.O. Lubchenco, C. Hansman, and E. Boyd, Pediatrics, 1966, 37(3), 403-416. Copyright 1966 by the American Academy of Pediatrics.
Reprinted with permission.
This form may be reproduced. The March of Dimes Birth Defects Foundation, 1982.
Next: Course Test |